Sinusitis
Condition Basics
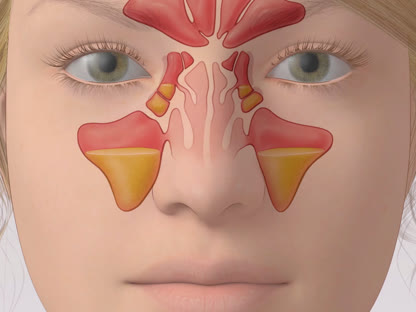
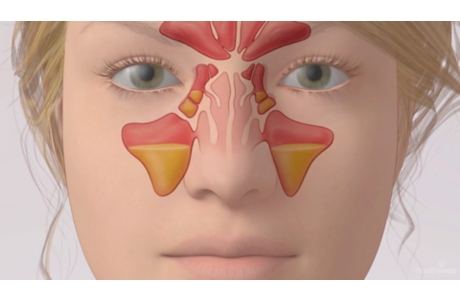
Sinusitis is an inflammation of the mucous membranes inside the nose and sinuses. Symptoms of sinusitis include pain in the face, a stuffy nose, and drainage from the nose. Sinusitis can be either acute (short-term) or chronic (long-term). Sinusitis is chronic when it lasts 12 weeks or more.
What causes it?
The cause of sinusitis varies depending on which type you have. Acute sinusitis is mainly caused by viruses but can also be caused by bacteria. The cause of chronic sinusitis may not be known, or it may be related to allergies, infections, or nasal polyps.
What are the symptoms?
Symptoms include pain and pressure in the head and face along with a stuffy or blocked nose. Other symptoms include drainage from the nose or down the back of the throat, a reduced sense of smell, ear pain, and tooth pain. Children often also have a cough.
How is it diagnosed?
Your doctor will ask about your current symptoms and how long you've had them. The doctor will also do a physical exam. You probably won't need any other tests if you have acute sinusitis. But you may need more tests if treatment doesn't help, if you have chronic sinusitis, or if you have complications.
Treatment depends on if you have acute or chronic sinusitis. A steroid nose spray along with a saline nose wash may relieve symptoms. If you have a bacterial infection, you may take antibiotics. Other medicines may be used. Surgery may be needed when sinusitis is chronic or severe and doesn't get better with medicines.
Cause
Acute sinusitis (short-term) is usually caused by a virus, but it can sometimes be caused by bacteria. When the mucous membranes inside the nose and sinuses get inflamed from a viral infection like a cold, they swell and make more mucus. This can block the normal drainage of fluid from the sinuses into the nose and throat. If the fluid and mucus can't drain, they build up over time. Bacteria may start to grow in them. These bacterial infections can cause more swelling and pain.
Sinusitis is called chronic (long-term) if the inflammation of the nose and sinus tissues lasts more than 12 weeks. Anything that causes the nose and sinuses to be inflamed for a long time can cause chronic sinusitis. This includes allergies and nasal polyps. A deviated nasal septum can also make it worse.
Learn more
Prevention
There are several ways you may reduce your chance of getting sinusitis.
- Treat stuffiness (nasal congestion) caused by colds or allergies promptly.
This can help you prevent an infection from developing in your sinuses.
- Avoid contact with people who have colds and other upper respiratory infections.
- Wash your hands often if you have contact with people who have colds or infections.
- Avoid cigarette, cigar, and pipe smoke in your home and workplace.
Smoke causes and further irritates inflamed membranes in your nose and sinuses.
- Avoid the things that trigger your allergy attacks if you have allergies.
Consider talking to your doctor about immunotherapy, such as allergy shots.
- Avoid breathing dry air.
Consider using a humidifier at home and work to increase the moisture in the air. Follow the directions for cleaning the machine.
Learn more
Watch
Symptoms
Symptoms include pain and pressure in the face along with a stuffy or blocked nose. Other symptoms include drainage from the nose or down the back of the throat. Leaning forward or moving your head may increase the pain in your face.
Other common symptoms of sinusitis may include:
- A headache.
- Pain or pressure in the ears.
- A cough.
- A fever.
- Tooth pain.
- A reduced sense of smell.
- Bad breath.
What Happens
There are two main types of sinusitis: acute (short-term) and chronic (long-term). Acute sinusitis often develops after a cold or viral infection. Swelling, inflammation, and a buildup of mucus caused by the cold can block the normal drainage of the nose and sinuses. This makes it easier for germs like viruses and bacteria to grow in the sinuses. Most sinus infections get better on their own. But antibiotics may be needed if there is a bacterial infection.
When inflammation in the sinuses lasts 12 weeks or longer, it is called chronic sinusitis. Anything that causes the sinuses to become inflamed and stay inflamed can lead to chronic sinusitis. This includes nasal allergies and nasal polyps that block the nasal passages or reduce drainage from the nose and sinuses. A deviated nasal septum can also make it worse.
When to Call a Doctor
Call your doctor now or seek immediate medical care if:
- You have new or worse swelling, redness, or pain in your face or around one or both of your eyes.
- You have double vision or a change in your vision.
- You have a high fever.
- You have a severe headache and a stiff neck.
- You have mental changes, such as feeling confused or much less alert.
Call your doctor if:
- Your symptoms of acute sinusitis do not improve after 10 days of home treatment.
- Your acute sinusitis symptoms start to get better within 10 days but then get worse again.
- You are not feeling any better within 5 to 7 days after starting antibiotics for a sinus infection.
- You have chronic sinusitis and you are not getting better as expected, or you have new symptoms of an acute sinus infection.
Watchful waiting
Watchful waiting is okay if you have symptoms of an early sinus infection (such as pain and pressure in your head along with a stuffy or runny nose). An early sinus infection can often be treated at home. If you develop symptoms of a sinus infection, start home treatment. This includes drinking lots of fluids and using saline nasal washes. Check the symptoms above to decide whether you need to call a doctor.
Check your symptoms
Exams and Tests
Your doctor can tell if you have sinusitis by asking questions about your current symptoms and how long you've had them. The doctor will also do a physical exam. You probably won't need any other tests. But you may need more tests if medicine doesn't help or your symptoms are chronic (long-term). More tests are also needed if you have problems caused by an infection. Tests may include an endoscopic sinus exam (nasal endoscopy) or CT scan.
Your doctor may refer you to an ear, nose, and throat (ENT) specialist. This may be needed if you don't get better over time. An ENT specialist will take a closer look at your nasal passages and upper throat. If allergies could be causing your sinus problems, you may need to see an allergist (immunologist).
Watch
Treatment Overview
Treatment depends on if you have acute or chronic sinusitis. A steroid nose spray along with a saline nose wash may relieve your symptoms. If needed, over-the-counter medicine can help with pain and pressure. If you have a bacterial infection, you may also get antibiotics. Other medicines may also be used.
Surgery may be needed when sinusitis is chronic or severe and doesn't get better with medicines.
Learn more
Self-Care
- Use saline (saltwater) nasal washes. This can help keep your nasal passages open and wash out mucus and allergens.
- You can buy saline nose washes at a grocery store or drugstore. Follow the instructions on the package.
- You can make your own at home. Add 1 teaspoon of non-iodized salt and 1 teaspoon of baking soda to 2 cups of distilled or boiled and cooled water. Fill a squeeze bottle or a nasal cleansing pot (such as a neti pot) with the nasal wash. Then put the tip into your nostril, and lean over the sink. With your mouth open, gently squirt the liquid. Repeat on the other side.
- Try a steroid nasal spray. This is especially good for chronic sinusitis.
- If needed, take an over-the-counter pain medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve). Read and follow all instructions on the label.
- For acute sinusitis, try a decongestant nasal spray like oxymetazoline (Afrin). Do not use it for more than 3 days in a row. Using it for more than 3 days can make your congestion worse.
- If the doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
- Be careful when taking over-the-counter cold or flu medicines and Tylenol at the same time. Many of these medicines have acetaminophen, which is Tylenol. Read the labels to make sure that you are not taking more than the recommended dose. Too much acetaminophen (Tylenol) can be harmful.
- Breathe warm, moist air. You can use a steamy shower, a hot bath, or a sink filled with hot water. Avoid cold, dry air. Using a humidifier in your home may help. Follow the directions for cleaning the machine.
Learn more
Watch
Medicines
Certain medicines may be used to treat acute or chronic sinusitis. Your doctor will let you know which medicine can help treat the type of sinusitis you have. You may use more than one medicine. Medicines may include:
- Corticosteroids. They reduce inflammation in the nasal passages. Examples include fluticason (Flonase) and mometasone (Nasonex). Most of the time, they are used as a nasal spray.
- Decongestants. They reduce the swelling of the mucous membranes in the nose. Some examples are oxymetazoline (such as Afrin) and phenylephrine (such as Neo-Synephrine).
- Analgesics. They relieve pain. They include acetaminophen (such as Tylenol) and ibuprofen (such as Advil).
- Antibiotics. They are prescribed to treat sinusitis caused by bacteria if your symptoms don't go away with time and self-care. They may be prescribed when symptoms of acute sinusitis don't start to get better within 10 days or if symptoms get better before 10 days but then get worse again.
- Allergy medicines. They may be used to treat nasal allergies (allergic rhinitis) or nasal polyps.
Be safe with medicines. Read and follow all instructions on the label.
Learn more
Related Information
Credits
Current as of: September 27, 2023
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: September 27, 2023
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.