Endometrial Cancer Prevention (PDQ®): Prevention - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What is prevention?
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
To prevent new cancers from starting, scientists look at risk factors and protective factors. Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied.
General Information About Endometrial Cancer
Endometrial cancer is a disease in which malignant (cancer) cells form in the tissues of the endometrium.
The endometrium is the lining of the uterus. The uterus is part of the female reproductive system. It is a hollow, pear-shaped, muscular organ in the pelvis, where a fetus grows.
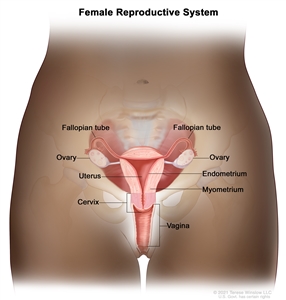
Anatomy of the female reproductive system. The organs in the female reproductive system include the uterus, ovaries, fallopian tubes, cervix, and vagina. The uterus has a muscular outer layer called the myometrium and an inner lining called the endometrium.
Cancer of the endometrium is different from cancer of the muscle of the uterus, which is called sarcoma of the uterus. See the PDQ summary on Uterine Sarcoma Treatment for more information.
See the following PDQ summaries for more information about endometrial cancer:
- Endometrial Cancer Screening
- Endometrial Cancer Treatment
Endometrial cancer is most common in postmenopausal women.
Endometrial cancer is diagnosed most often in postmenopausal women at an average age of 60 years.
Since the mid-2000s, the number of new cases of endometrial cancer has increased slightly each year. From 2015 to 2019, the number of deaths from endometrial cancer increased by about 1% per year.
Endometrial Cancer Prevention
Avoiding risk factors and increasing protective factors may help prevent cancer.
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight, and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
The following risk factors increase the risk of endometrial cancer:
Endometrial hyperplasia
Endometrial hyperplasia is an abnormal thickening of the endometrium (lining of the uterus). It is not cancer, but in some cases, it may lead to endometrial cancer.
Estrogen
Estrogen is a hormone made by the body. It helps the body develop and maintain female sex characteristics. Estrogen can affect the growth of some cancers, including endometrial cancer.
A woman's risk of developing endometrial cancer is increased by being exposed to estrogen in the following ways:
- Estrogen-only hormone therapy: Estrogen may be given to replace the estrogen no longer produced by the ovaries in postmenopausal women or women whose ovaries have been removed. This is called hormone therapy (HT). The use of HT that contains only estrogen increases the risk of endometrial cancer, and the risk grows higher the longer the estrogen is used. For this reason, estrogen therapy alone is usually prescribed only for women who do not have a uterus.
When estrogen is combined with progestin (another hormone), it is called combination estrogen-progestin therapy. For postmenopausal women, taking estrogen in combination with progestin does not increase the risk of endometrial cancer, but it does increase the risk of breast cancer. (See the Breast Cancer Prevention summary for more information.)
- Early menstruation: Beginning to have menstrual periods at an early age increases the number of years the body is exposed to estrogen and increases a woman's risk of endometrial cancer.
- Late menopause: Women who reach menopause at an older age are exposed to estrogen for a longer time and have an increased risk of endometrial cancer.
- Never being pregnant: Because estrogen levels are lower during pregnancy, women who have never been pregnant are exposed to estrogen for a longer time than women who have been pregnant. This increases the risk of endometrial cancer.
Tamoxifen
Tamoxifen is one of a group of drugs called selective estrogen receptor modulators, or SERMs. Tamoxifen acts like estrogen on some tissues in the body, such as the uterus, but blocks the effects of estrogen on other tissues, such as the breast. Tamoxifen is used to prevent breast cancer in women who are at high risk for the disease. However, using tamoxifen for more than 2 years increases the risk of endometrial cancer. This risk is greater in postmenopausal women.
Raloxifene is a SERM that is used to prevent bone weakness in postmenopausal women. However, it does not have estrogen-like effects on the uterus and has not been shown to increase the risk of endometrial cancer.
Obesity, weight gain, metabolic syndrome, and diabetes
Obesity, gaining weight as an adult, or having metabolic syndrome increases the risk of endometrial cancer. Obesity is related to other risk factors such as high estrogen levels, having extra fat around the waist, polycystic ovary syndrome, and lack of physical activity.
Having metabolic syndrome increases the risk of endometrial cancer. Metabolic syndrome is a condition that includes extra fat around the waist, high blood sugar, high blood pressure, and high levels of triglycerides (a type of fat) in the blood.
Having type 2 diabetes may increase the risk of endometrial cancer.
Genetic factors
Based on solid evidence, women with certain genetic conditions have an increased risk of developing endometrial cancer.
Lynch syndrome is an inherited disorder caused by changes in certain genes. Women who have Lynch syndrome have a much higher risk of developing endometrial cancer than women who do not have Lynch syndrome.
Polycystic ovary syndrome (a disorder of the hormones made by the ovaries), and Cowden syndrome are inherited conditions that are linked to an increased risk of endometrial cancer.
Women with a family history of endometrial cancer in a first-degree relative (mother, sister, or daughter) are also at increased risk of endometrial cancer.
The following protective factors decrease the risk of endometrial cancer:
Pregnancy and breast-feeding
Estrogen levels are lower during pregnancy and when breast-feeding. The risk of endometrial cancer is lower in women who have had children. Breastfeeding also decreases the risk of endometrial cancer.
Hormonal contraceptives
Taking hormonal contraceptives (birth control pills) that combine estrogen and progestin (combined oral contraceptives) decreases the risk of endometrial cancer. The protective effect of this type of birth control increases with the length of time they are used, and can last for many years after oral contraceptive use has been stopped.
While taking birth control pills, women have a higher risk of blood clots, stroke, and heart attack, especially women who smoke and are older than 35 years.
New data suggest that other hormonal contraceptives, such as birth control devices that are inserted into a woman's uterus, may also decrease the risk of endometrial cancer.
Weight loss
It is not known if losing weight decreases the risk of endometrial cancer. However, having bariatric surgery (a surgery that changes how your digestive system works so you will lose weight) decreases the risk of endometrial cancer. After bariatric surgery, other obesity-related conditions, such as diabetes and metabolic syndrome often improve or go away.
Having bariatric surgery also includes risks, such as infection, blood clots, breathing or heart problems, and digestive issues.
Physical activity
Physical activity (exercise) may lower the risk of endometrial cancer. This includes any physical activity you do at your job or at home.
It is not known if the following factors affect the risk of endometrial cancer:
Fruits, vegetables, and vitamins
A diet that includes, fruits, vegetables, phytoestrogen, soy, and vitamin D has not been found to affect the risk of endometrial cancer.
Taking multivitamins has little or no effect on the risk of common cancers, including endometrial cancer.
Hair products, including dyes, bleach, highlights, straighteners, and permanents
There is not enough evidence to show a link between hair products and endometrial cancer. One retrospective study discussed a possible link between certain hair products and uterine cancers, including endometrial cancers.
Cancer prevention clinical trials are used to study ways to prevent cancer.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials are conducted with healthy people who have not had cancer but who have an increased risk for cancer. Other prevention trials are conducted with people who have had cancer and are trying to prevent another cancer of the same type or to lower their chance of developing a new type of cancer. Other trials are done with healthy volunteers who are not known to have any risk factors for cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines, vitamins, minerals, or food supplements.
New ways to prevent endometrial cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about endometrial cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Endometrial Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/uterine/patient/endometrial-prevention-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389201]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2023-08-21
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

